2026 ADA Standards of Care in Diabetes
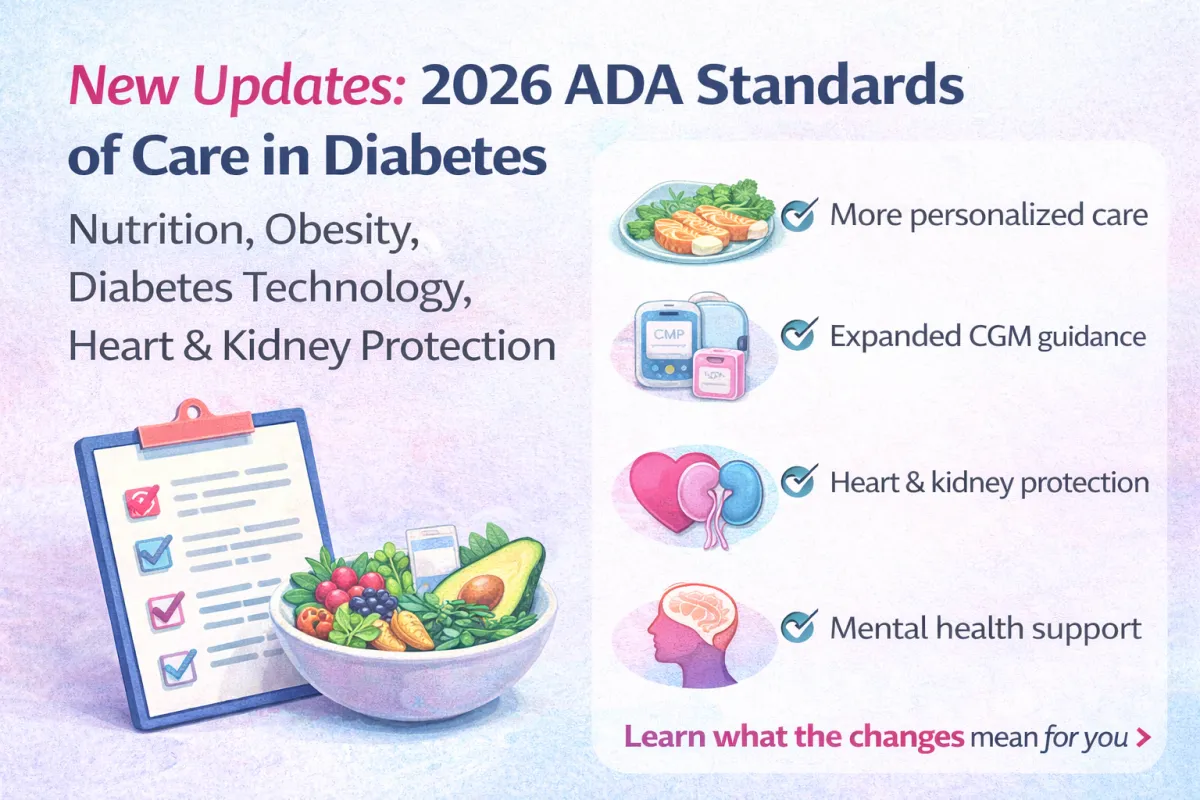
2026 ADA Standards of Care in Diabetes Updates Overview
Every year, the American Diabetes Association (ADA) updates its Standards of Care in Diabetes. These updates matter because they help guide doctors, pharmacists, diabetes educators, and people living with diabetes toward the safest and most effective care.
The 2026 Standards of Care include important updates in several key areas, including:
Nutrition and obesity treatment support
Diabetes technology like CGMs and insulin pumps
Heart and kidney protection
Diabetes care in the workplace and school
Screening and monitoring updates
Special situations like pregnancy, cancer treatment, and organ transplant
This blog post gives you a clear overview of what’s new—and what it may mean for people living with diabetes.
Important note: This blog is for education only and does not replace medical advice. Always talk with your healthcare provider before making changes to medications or devices.
1) Big Picture Shift: More Personalized Diabetes Care
One of the strongest themes in the 2026 ADA Standards is this:
✅ Diabetes care should be personalized, not “one-size-fits-all.”
The ADA continues to emphasize shared decision-making, which means:
You and your healthcare team make decisions together
Your goals, preferences, finances, and lifestyle matter
Your treatment plan should fit your real life
This is a major step forward, because people do better when their plan is realistic and sustainable.
Why this matters:
When people feel heard and supported, they are more likely to stay consistent with nutrition changes, medication routines, and glucose monitoring.
Reference: ADA Standards of Care in Diabetes—2026
2) Nutrition + Obesity Care: More Support, Not Just “Eat Less”
The ADA continues to recognize that obesity is not about willpower alone. It is a medical condition influenced by:
hormones
stress
sleep
medications
metabolism
environment
mental health
food access and affordability
One of the updated messages in 2026 is that weight management plans should include:
✅ nutrition support
✅ physical activity
✅ behavioral health support
✅ counseling
✅ regular monitoring
This is important because many people have tried diets and failed—not because they are lazy, but because they didn’t have enough structure or support.
What aligns with functional medicine?
This is actually very aligned with functional medicine because it supports:
whole-person care
root-cause thinking
stress and sleep as key drivers
behavior change support
Reference: ADA Standards of Care in Diabetes—2026
3) Stronger Focus on Heart and Kidney Protection
Diabetes is not only about A1C. It is also about preventing long-term complications, especially:
heart disease
stroke
chronic kidney disease (CKD)
The 2026 Standards continue to highlight medications that can reduce these risks, including:
SGLT2 inhibitors
These are often used to help:
slow kidney disease progression
reduce cardiovascular risk in appropriate patients
GLP-1 receptor agonists
These may support:
weight loss
improved blood sugar control
cardiovascular risk reduction
The ADA is continuing to refine guidance about how these medications are used in more complex situations (like kidney disease and dialysis), because many people with type 2 diabetes also have kidney and heart conditions.
Why this matters:
This supports a more prevention-focused approach instead of waiting until complications happen.
Reference: ADA Standards of Care in Diabetes—2026
4) New Guidance for Special Situations (Cancer, Transplant, Surgery)
Some of the 2026 updates include medication guidance for diabetes management in special cases, such as:
people receiving certain cancer treatments
people who have had an organ transplant
people having surgery (peri-operative care)
This matters because diabetes care can become more complicated when someone is dealing with:
steroids
immune therapies
transplant medications
stress hormones from surgery or illness
The ADA highlights the need for careful glucose monitoring and safe medication choices in these situations.
Reference: ADA Standards of Care in Diabetes—2026
5) Diabetes Technology Updates: CGMs Are Expanding
One of the biggest and most exciting updates is around continuous glucose monitoring (CGM).
The ADA now recommends CGM more broadly, including:
✅ CGM can be used at diabetes diagnosis or any time after
✅ CGM may be used for people on insulin
✅ CGM may be helpful for people using medications that can cause hypoglycemia
✅ CGM may be useful to support management across many treatment plans
The 2026 Standards also recognize different types of CGM options, including:
real-time CGM (rtCGM)
professional CGM (clinic-owned, short-term use)
over-the-counter CGM (OTC CGM), where available
Why CGM is such a big deal for diabetes
CGM can help people see patterns like:
morning high fasting glucose
food-related spikes
stress-related spikes
nighttime lows
exercise responses
And it helps move diabetes care away from “guessing” and toward data-driven decisions.
Reference: ADA Standards of Care in Diabetes—2026
6) Insulin Pumps and Automated Insulin Delivery: Fewer Barriers
Another update in 2026 is that the ADA is removing certain barriers to starting advanced insulin technology, such as:
not requiring C-peptide testing
not requiring specific antibody testing
not requiring a certain insulin duration before starting pump or automated delivery systems
Why this matters:
This can help more people access the tools they need without unnecessary delays.
Reference: ADA Standards of Care in Diabetes—2026
7) Safety and Support: Workplaces and Schools Matter
The ADA also continues to emphasize that diabetes care doesn’t only happen at home or in a clinic.
People need support in real life settings, including:
Workplace accommodations
If someone uses diabetes technology, they may need:
time to check glucose
time to treat lows
time to calibrate or troubleshoot devices
time to eat snacks or meals safely
School support for children and teens
Students using devices like:
CGM
insulin pumps
connected insulin pens
automated insulin delivery systems
may need additional support at school for safe diabetes management.
Reference: ADA Standards of Care in Diabetes—2026
8) Tobacco and Vaping: Stronger “Avoid” Messaging
The ADA continues to advise avoiding tobacco products and also highlights the importance of avoiding:
e-cigarettes
vaping
This is important because nicotine use is linked with:
higher cardiovascular risk
increased inflammation
worse diabetes outcomes
If someone wants to quit, the ADA supports treatment that includes:
counseling
medications when appropriate
Reference: ADA Standards of Care in Diabetes—2026
9) Updated Monitoring and Screening Recommendations
The ADA includes updates around monitoring important health markers, including:
kidney function tests (eGFR)
potassium levels for certain blood pressure and kidney medications
blood pressure goals
anxiety screening
diabetes distress and mental health support
This matters because diabetes management is not only physical—it’s emotional too.
Diabetes distress is real, and support matters.
Reference: ADA Standards of Care in Diabetes—2026
10) Pregnancy Updates: More Detailed Guidance
The 2026 Standards include updated guidance for diabetes management in pregnancy, including topics like:
preconception planning
weight and glucose goals
CGM use
insulin options
blood pressure and triglyceride management
Pregnancy with diabetes requires a very careful plan, and the ADA continues to improve clarity in this area.
Reference: ADA Standards of Care in Diabetes—2026
What These Updates Mean for YOU (Simple Takeaways)
If you’re living with diabetes, here are the most helpful takeaways:
✅ You deserve a plan that fits your life
Shared decision-making matters. Your lifestyle and stress level matter.
✅ You don’t have to do this alone
Nutrition and obesity treatment should include support, not shame.
✅ Technology is becoming more accessible
CGM is being recommended for more people—not just those on insulin.
✅ Diabetes care is about prevention
Protecting your heart and kidneys is just as important as A1C.
✅ Your mental health matters too
Anxiety screening and diabetes distress support are now part of better care.
Final Thoughts
The 2026 ADA Standards of Care show that diabetes care is evolving in a good direction:
More personalized.
More supportive.
More focused on prevention.
More focused on quality of life.
And that is exactly what people with diabetes need.
If you want help creating a simple, realistic plan to improve your blood sugar, weight, and energy—without extreme dieting—this is what we do inside Rx Health & Wellness.
References (Real + Reliable)
American Diabetes Association. Standards of Care in Diabetes—2026. Diabetes Care. (2026).
(Official ADA Standards publication—use the final published link from ADA when available.)American Diabetes Association. Diabetes Technology: Standards of Care in Diabetes. Diabetes Care. (Updated annually)
https://diabetesjournals.org/careNational Institute of Diabetes and Digestive and Kidney Diseases (NIDDK). Diabetes Overview and Management
https://www.niddk.nih.gov/health-information/diabetesCenters for Disease Control and Prevention (CDC). Diabetes and Heart Disease Risk
https://www.cdc.gov/diabetesU.S. Preventive Services Task Force (USPSTF). Behavioral Counseling and Preventive Recommendations
https://www.uspreventiveservicestaskforce.org/
