
Do I Have to Check My Blood Sugar?
Do I Have to Check My Blood Sugar?
One of the most common questions people with type 2 diabetes ask is:
“Do I really have to check my blood sugar every day?”
Let’s be honest — many people don’t like pricking their fingers. It can be uncomfortable, inconvenient, and even emotionally draining. But before you toss your glucometer in a drawer, let’s explore what the science actually says — and when checking truly matters.
What the Research Says
A landmark study published in JAMA Internal Medicine (Young et al., 2017) followed adults with type 2 diabetes not using insulin. Participants were divided into three groups:
No self-testing
Once-daily testing
Once-daily testing with feedback messages
After one year, researchers found no significant difference in A1C or quality of life between groups.
👉What that means:
For many people with type 2 diabetes not using insulin, daily finger-stick checks may not improve long-term glucose control.
📚Reference:
Young LA, et al.JAMA Intern Med. 2017;177(7):920–929.
Study Summary – American Medical Association
When Checking Blood Sugar Does Help
Even though daily testing may not be necessary for everyone, there are times when it’s incredibly valuable, such as:
When starting or adjusting medications
If your A1C is above target and you need more real-time data
To understand how specific foods, stress, or exercise affect you
During illness, infection, or poor sleep
When you feel unusual fatigue, dizziness, or mood changes
🩺 Checking your blood sugar provides immediate feedback— empowering you to connect choices with outcomes.
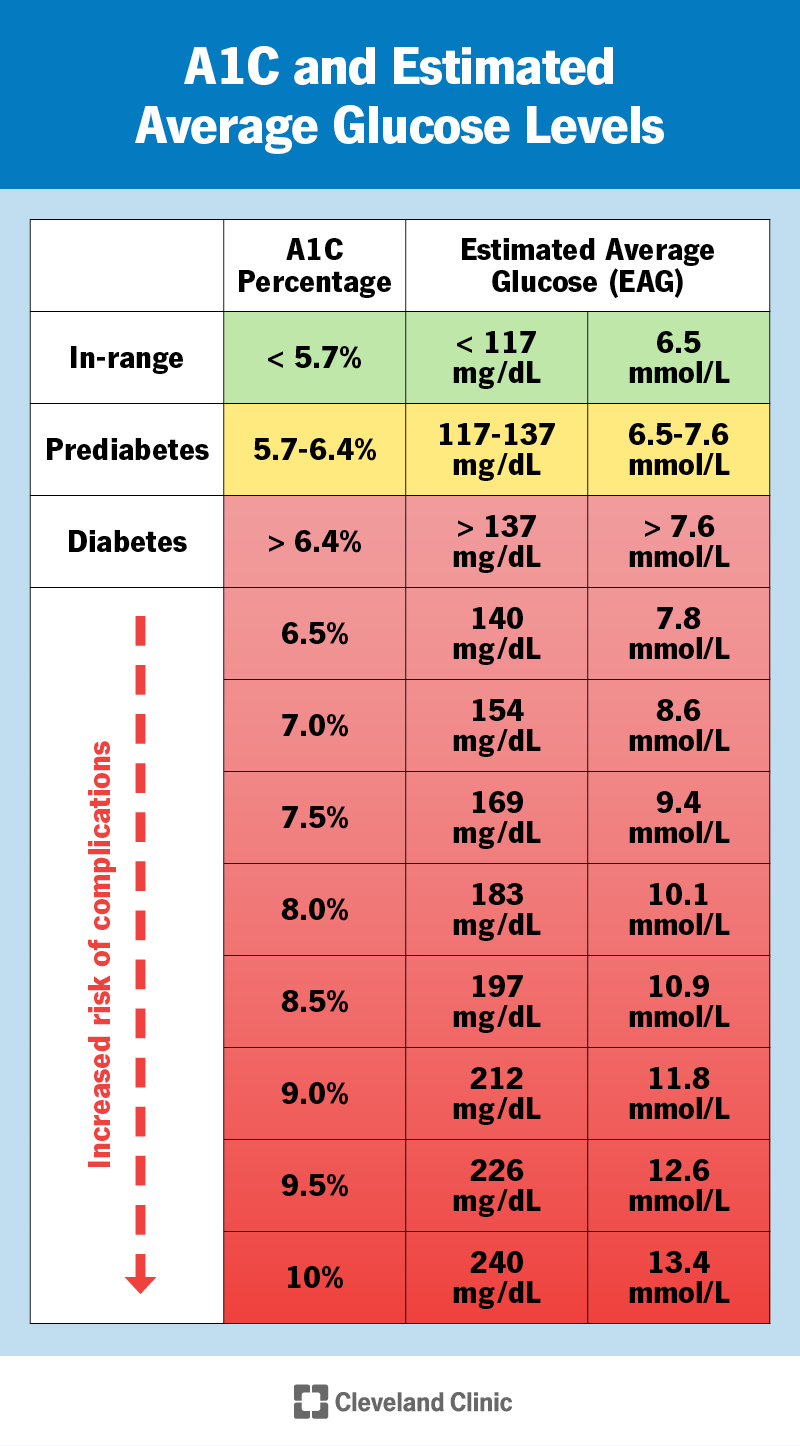
Why A1C Isn’t Enough
A1C gives an average blood sugar over 2–3 months, but it hides the daily fluctuations that matter most for preventing complications.
It won’t show:
Morning fasting highs (the “Dawn Effect”)
Post-meal spikes
The impact of stress or lack of sleep
Low blood sugars after exercise or skipped meals
That’s why occasional self-monitoring (or CGM use) can complement A1C testing — helping you see patterns and make better daily decisions.
Knowledge Is Power
Testing shouldn’t feel like punishment — it’s information. When used intentionally, it helps you:
Identify which meals cause glucose spikes
See how movement lowers your numbers
Understand how sleep and stress affect blood sugar
Know when to talk with your healthcare provider about medication changes
🔎 According to a Cochrane Review (2012), self-monitoring improves A1C— especially when people use the data to adjust behavior or treatment.
(Cochrane Database Syst Rev. 2012;(1):CD005060)
If You Use Insulin, Testing Is Essential
If you take insulin, especially mealtime or rapid-acting types, testing isn’t optional — it’s a safety tool.
Monitoring helps you:
Avoid hypoglycemia (low blood sugar)
Adjust doses safely during illness or stress
Time meals and exercise correctly
Prevent long-term complications
Continuous Glucose Monitors (CGMs): A Better Way
If finger sticks frustrate you, consider a Continuous Glucose Monitor (CGM)— a small wearable sensor that tracks glucose 24/7.
CGMs can:
Send data to your phone or smartwatch
Alert you to highs and lows
Show trends, not just single readings
Reduce anxiety about unexpected drops
In fact, the International Consensus on Time in Range (Battelino et al.,Diabetes Care, 2019) confirms that CGMs significantly improve glucose control and quality of life for people with both Type 1 and Type 2 diabetes.
🧭So… Do You Have to Check?
Not necessarily — but you should check with purpose.
If you’re on oral medication only and your A1C is stable, less frequent checks might be fine.
But if you’re adjusting your plan, exploring food triggers, or using insulin, monitoring offers valuable insight that helps you take control of your health.
Better understanding = Better control = Better outcomes.
References
Young LA, et al.JAMA Intern Med. 2017;177(7):920–929.
Farmer A, et al.Cochrane Database Syst Rev. 2012;(1):CD005060.
Battelino T, et al.Diabetes Care. 2019;42(8):1593–1603.
American Diabetes Association.Standards of Care in Diabetes – 2024.
Mayo Clinic:How to use a blood glucose meter
